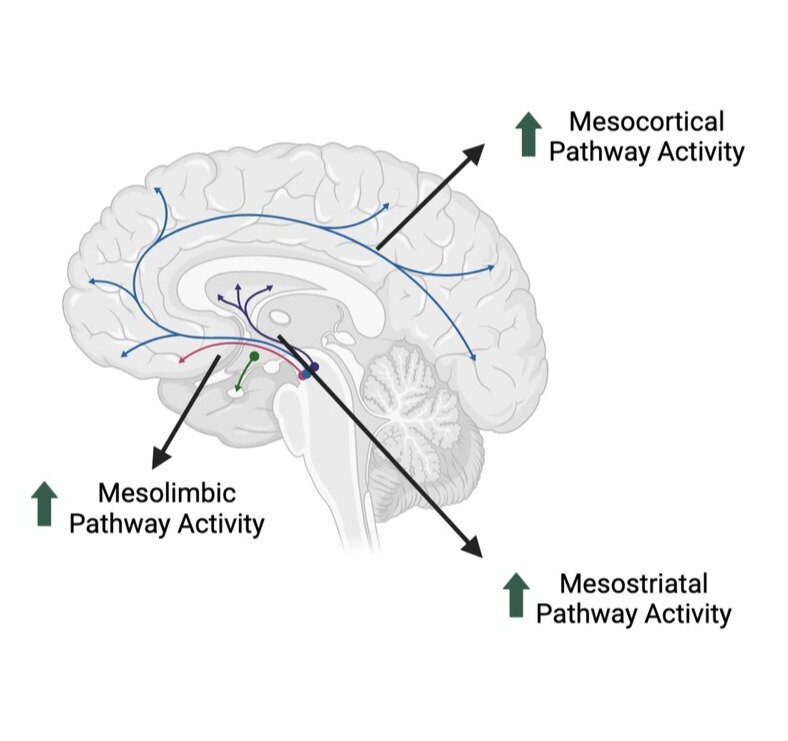
Obesity represents one of the main global health challenges of the 21st century, being associated with numerous comorbidities, including cardiovascular diseases, diabetes, and different forms of cancer. Although lifestyle modifications remain the cornerstone of treatment, their long-term adherence is often limited, while more invasive interventions, such as bariatric surgery, carry risks and are appropriate only for selected categories of patients. This makes it necessary to explore alternative therapeutic approaches. In this context, growing attention is being paid to drugs capable of modulating the dopaminergic reward system, potentially useful in controlling appetite and eating behaviors. Methylphenidate (MPH), commonly used in the treatment of ADHD, increases synaptic availability of dopamine and noradrenaline and could influence the hedonic regulation mechanisms of food intake. Methods Results Discussion Conclusion
This narrative review evaluated the effect of methylphenidate on appetite, body weight, and anthropometric parameters in overweight or obese adults. Through a PICO approach, 39 studies were selected (14 RCTs and 3 observational).
Methylphenidate was found to be associated with a modest weight loss (about 1–2%) and significant appetite suppression. The effects appear more evident in women, while in men the evidence is less consistent, probably due to limitations in statistical power.
Although MPH shows potential as an additional pharmacological option in the management of obesity, important questions remain regarding cardiovascular safety, sustainability of effects, and gender-differentiated response. The methodological heterogeneity of the studies, small sample sizes, and lack of long-term follow-up limit the generalizability of the results.
Methylphenidate appears able to suppress appetite and reduce caloric intake, with a more pronounced effect in women. However, current evidence is not sufficient to recommend its clinical use in obesity management. Large-scale randomized studies with prolonged follow-up, structured safety assessment, and gender-stratified analyses are needed, as well as investigations into possible associations with lifestyle interventions or other pharmacological therapies.


©

Effetti anoressizzanti del metilfenidato
Effetti anoressizzanti del metilfenidato
2025-12-28 15:21
2025-12-28 15:21
Array() no author 90785
Obesità, adhd, dopamina, obesita, microbiotaedintorni, appettito, ricompensa, noradrenalina,

©